Ligamentum arteriosum also called the arterial ligament.It refers to the small ligament that connects the upper surface of the proximal descending aorta with the left pulmonary artery in your heart.
It is in a non-functional form of the ductus arteriosus, and it forms around the third week after birth.
You might think that it does not amount to any complications, but it does.
In this article, we will discuss its anatomy and the possible complications and their solutions.
Table of Contents
Ductus Arteriosus And Ligamentum Arteriosum

i. Placenta
During the intrauterine phase, the fetus gets oxygen and the essential nutrients from the mother’s blood circulation. The main organ through which the exchange takes place is the placenta.
The placenta is a unique organ present only during pregnancy. It is also an organ considered to be formed by two entirely different bodies. It is because it has a fetal and a maternal surface to it.
In the villi of the placenta, oxygen and essential nutrients are released from the mother’s blood, and they are transferred to fetal blood. Thus, enabling the fetus to get all the elements needed for life.
This exchange happens with either minimum or no direct contact between these two circulations. Only a small number of cells passes through this, but this amount rarely causes any problems. One of them can be the Rh incompatibility.
ii. Fetal Circulation
Considering the fact that there is no breathing during an intrauterine phase, there is no need for blood to circulate through the lungs. To bypass the lungs, there needs to be a connection between the pulmonary and systemic circulation.
This particular nexus or connection is formed by the ductus arteriosus. It is a part-time blood vessel that connects the aorta to left pulmonary artery. This helps to direct all the blood from the pulmonary artery to flow into the aorta instead of lungs.
All of this results in the blood to flow through the fetal body without any problems while bypassing the lungs.
iii. Ligamentum Arteriosum
After the birth of a baby, during the first breathe the lungs expand, causing the blood to start circulating from the right ventricle of the heart through the pulmonary artery and then finally into the pulmonary circulation.
That forms the only way for the body to get required amounts of oxygen and nutrition since the connection to the mother’s circulation is now disconnected.
The expansion of lungs causes bradykinins to be released into the baby’s circulation. These changes cause the ductus arteriosus to eliminate in some time.
Approximately after three weeks, obliterated ductus turns into a sort of a connective tissue and changes its name to ligament arteries.
Once it is completely eliminated, ligament doesn’t have anymore lumen. This causes the circulation of blood impossible.
But, unfortunately, this physiological process does not always come to an end, and it does not get eliminated. This causes PDA (Persistent Ductus Arteriousus), and it has to be treated surgically during infancy.
Anatomy Of Ligamentum Arteriosum
Since ligament arteriosum is the postnatal form of the ductus, its location is the same as one of the ductus arteriosus. It is located on the upper surface of the proximal descending aorta connecting it to the pulmonary artery on the left.
Ligamentum arteriosum lies horizontally while the left recurrent laryngeal nerve arches right around it. Heart plexus, in particular, its shallow sections, is located in front of ligamentum arteriosum.
Heart plexus corresponds to a tangle of nerves responsible for innervating the heart from its base. Deeper towards the right lies the left main bronchus.
Vagus Nerve
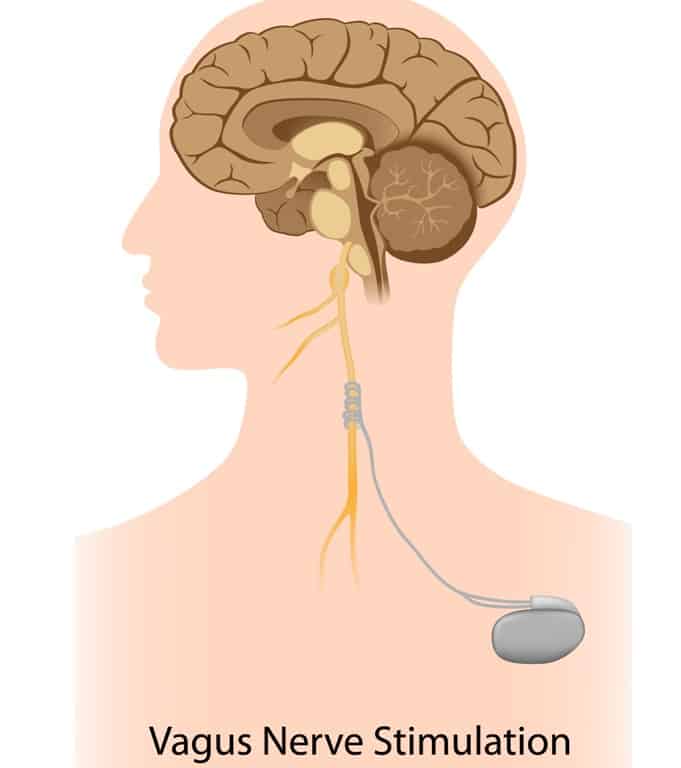
Cranial nerves are the pairs of the nerves that origin from different centers located inside your brain collectively. These nerves are responsible for motor and sensitive innervations of the various structures in your body.
There are 12 pairs of cranial nerves, and the tenth one is called Vagus Nerve. It is also called Cranial Nerve X sometimes.
The Phrenic Nerve typically originates from the 4th cervical nerve and is located in the front of the ligament.
When Ductus Arteriosus Fails To Close?
Normally, ductus arteriosus begins to close within twelve to twenty-four hours after the birth. As the baby starts breathing independently, the pulmonary artery opens and allows the blood to enter the lungs.
This essentially prompts the ductus arteriosus to close. When the ductus arteriosus doesn’t close after birth, this condition known as Patent Ductus Arteriosus (PDA).
In patent ductus arteriosus, oxygenated blood from the aorta mixes with the deoxygenated blood from the pulmonary artery. This adds to the amount of blood flowing into the lungs.
This consequently puts a strain on the heart and increases the blood pressure of the lung. This condition is called pulmonary hypertension.
PDA affects girls, newborns and premature infants with neonatal respiratory distress syndrome. Neonatal respiratory distress syndrome is a condition that is seen to lower oxygen supply due to premature lungs.
The doctors might not be able to diagnose this at first and discover it until later in childhood or adulthood. It is because the PDA is too small. Sometimes, doctors discover it while they detect heart murmurs (a whooshing or a swishing sound).
Symptoms Of Infancy Or Childhood PDA
a. Poor appetite
b. Breathlessness
c. Fast heartbeat
d. Recurrent respiratory infections
e. Tiring more easily
f. Poor growth
g. If the PDA is small, treatment is not necessary. If it’s large, you must seek medical attention to prevent any serious complications, like endocarditis or heart failure.
The possible medical treatments include surgery, nonsteroidal anti-inflammatory drugs (NSAIDs), and cardiac catheterization.
h. Surgery, like thoracotomy, is the standard selection of treatment of PDA. The aim is to repair the affected area to prevent the lungs from any damage due to the increased blood pressure.
The surgery also helps you to restore the proper pattern of blood flow. Thoracotomy enables the surgeons to gain access to certain organs, like your heart, by cutting open your chest.
The common complications of this surgery are infections, a respiratory failure, air leaks, and bleeding.
i. Indomethacin and Ibuprofen are examples of NSAIDs that can be used in premature infants to constrict the ductus arteriosus. These drugs won’t work for adults, children, or newborns.
Monitoring or observing is the only solution for adults, children, and newborns with small PDA that is not causing any major health problems.
j. Cardiac catheterization is a procedure using a thin, flexible tube that goes up to a blood vessel in the groin that in turn leads to your heart. Through this tube, the doctor introduces a coil that helps close the ductus arteriosus.
k. Doctors do not usually perform the cardiac catheterization on premature infants because they are fragile and too small.
If a newborn does not experience health problems associated with the open ductus arteriosus, the doctors wait until the newborn is a little older to perform this procedure.
l. Doctors recommend mothers to feed their baby with a high-calorie formula or unadulterated breast milk in order to promote proper growth.
If a baby does not tolerate oral feedings, the food goes through a small, flexible tube that goes through the nose and down to the stomach. The intake of fluids might be restricted.
Complications With Ligamentum Arteriosum
When the ductus arteriosus eventually becomes ligamentum arteriosum, it becomes completely non-functional. However, this ligament plays a major role in severe injuries and a few heart abnormalities.
It helps control the aortic arch, which generally supplies blood to the neck arms region and the head, during the different steps of the cardiac cycle.
1. Traumatic Aortic Tear
A traumatic aortic tear is usually always fatal because of the profuse bleeding. Around 18 percent of deaths that happen due to vehicular accidents are a result of this injury.
One of the reasons that make this injury a fatal one is the tearing of the aorta due to ligamentum arteriosum. This ligament fixes the aorta in place when it goes back to its normal position after any rapid deceleration, causing a partial or a complete aortic tearing.
During any abrupt deceleration—such as in a car crash—the heart shifts towards the front of your chest. As the ligamentum arteriosum is holding the aorta in its place it’s movement is restricted.
As a result, the powerful force of the motion overstretches the said ligament. In most of the cases, it leads to massive blood loss and death.
Mediastinal hematoma might also occur in partial aortic tear that happens near the ligamentum arteriousum. This type of an injury causes blood to pool in the middle section of your chest called the mediastinum.
The goal of the treatment for a traumatic aortic tear is to control the heart rate and the blood pressure and an immediate surgical repair.
However, more and more doctors are now using endovascular stent, which is used to place a small wire-mesh tube in the affected artery. In some cases, they might perform this procedure along with surgical repair of the affected artery.
2. Vascular Ring
Vascular ring is a congenital abnormality of the aorta, the largest blood vessel carrying oxygen-rich blood out of our heart.
It involves the ligamentum arteriosum, the pulmonary artery, and left subclavian artery.
The most common type of vascular ring is a double aortic arch, followed by a right-sided aortic arch with left ligamentum arteriosum.
There are two types of vascular ring: The partial vascular ring and then, the complete vascular ring (sometimes called the double aortic arch). In a complete vascular ring, the aorta or its branches enclose the windpipe and the.
A right-sided aortic arch generally affects adults and it is associated with certain congenital heart abnormalities. It doesn’t cause any such symptoms unless there’s an artery enlargement (aneurysm).
In healthy individuals, the aorta bends to their left and then passes at the front and then the left side of the windpipe.
The ligamentum arteriosum attaches the descending aorta to the left pulmonary artery. In the right-sided aortic arch, the aorta simply bends to the right.
This results in the left subclavian artery to completely encircle the windpipe. The situation becomes even worse when the ligamentum arteriosum constricts the windpipe.
Symptoms of vascular ring show up within the first few weeks or months of life. In some children, they only have symptoms as adults when the arteries harden (atherosclerosis).
Children or an infant may suffer from the following symptoms:
- Difficulties in breathing or swallowing
- Constant discharge (if the esophagus is constricted)
- Vomiting
- Shallow breaths or long pauses while breathing or sleeping
- Recurrent respiratory infections
- Poor weight gain and growth
- Feeding difficulties
The only way to treat vascular rings is through surgery. This usually involves a tiny incision on the left of your chest in between the ribs. The main purpose of the surgery is to tear apart the vascular ring to relief the pressure off your windpipe and esophagus.
If a qualified surgical team performs the surgery, it’s usually safe. This eases the symptoms immediately.
You need not follow any special diet after the surgery. You only need to take a few painkillers post surgery.
Vascular rings are usually not fatal if the doctor diagnoses it early. However, infants and children might still experience severe breathing problems for months.
If you do not undergo surgery, this condition might complicate and cause even more severe symptoms. Sudden death is a possibility.
3. Calcification Of The Ligamentum Arteriosum
Calcium plays a significant role in the pumping of your heart. Accumulation of calcium in the heart is harmless.
But, in certain situations, it could hint at an underlying health problem. For example, calcium deposits might lead to the hardening of your heart tissues and thereby cause heart failure.
The study shows that calcification of the ligament arteriosum is a very common and normal finding among adults and children.
Calcification of this ligament becomes more common as you age and with the presence of atherosclerosis.
Atherosclerosis is the compound that is responsible for hardening of the major blood vessels. In children, parents should not confuse this with any disease process.
It commonly occurs within a couple of months or years after your child’s ductus arteriosus closes.
It isn’t clear what the clinical implication of this findings are because of conflicting studies. Nevertheless, calcification of the ligament arteriosum might serve as proof that the ductus arteriosus has closed in asymptomatic children.
There are no standard medications for fixing this condition since it is considered normal and harmless. However, you must go for regular checkups just to be sure that you and your baby are not suffering from any health problems.
Treatment For Ligamentum Arteriosum
The objective of treating a PDA is to close the blood vessel. Thus allowing a normal blood supply to the body. There are mainly three ways to which doctors can close the PDA.
The choice of method depends on the size of the opening and the effect it has on the body. If the opening is small and the blood flow is not that abnormal, management of the symptoms can be an option.
In some cases, the opening might even close on its own. In case the opening is large, and blood flow is abnormal, more invasive methods, which include medication and surgery, might be used.
1. PDA Management And Spontaneous Closure
If a PDA is small and it is not interfering with your blood flow to any great extent, waiting for spontaneous closure is a good option. The majority of the babies born with a PDA fit into this asymptomatic kind.
The PDA will close within a few days under normal circumstances. It might be that the premature baby requires extra time for the PDA to close on its own. Spontaneous closure is common, especially for babies who are mildly premature.
Trained staff in the Neonatal Intensive Care Unit (NICU) will control fluids to prevent an excessive blood flow to the lungs.
This is done ensuring enough blood flow to the vital organs in the body. A disproportionate volume of fluid may cause too much blood flow, not letting the PDA close.
2. Drug Therapy For PDA
If the PDA does not close on its own or if it is large, drug therapy is used to encourage a PDA to close. In the womb, the ductus arteriosus is bound to stay open.
The placenta is a source of a substance known as prostaglandin E 2. This is responsible for preventing the artery from closing.
Indomethacin is prescribed if the PDA remains open after birth. Indomethacin inhibits the effect of prostaglandin E 2. It is effective if it is given within the first two weeks after birth.
Indomethacin might also have a few have side effects. These essentially include bleeding, infection, and a few other longer-term complications.
If it is administered rapidly, it might cause a drop in the blood flow to the kidneys and bowel. Slow administration of this medication will help you avoid these complications.
Indomethacin sometimes causes the platelets in the blood to become less sticky. This increases the risk of bleeding. For premature babies with normal platelet count, this is not usually a problem.
3. Surgery For PDA
If drug therapy fails or is not an option, surgery can be performed. Surgical ligation is considered to be a low-risk procedure and is successful in almost all cases, even for premature babies.
The surgery can be performed in the traditional manner,i.e., an open heart surgery, or with a thin tube known as a catheter.
The method that will be used to close the ductus arteriosus depends on the size of the opening, again. Sometimes sewing up the opening is enough.
At other times a tiny patch may be sewn above the opening from the inside of your heart.
Although the success rate for this surgery is very good, it might lead to deformities in the heart. The baby might become unstable for 24 to 48 hours after the surgery.
Some babies might require ventilator support or treatment for heart failure with low blood pressure.
Other complications of the surgery are pretty rare. There might be bleeding, damage to a blood vessel, nerve damage or infection.
Final Talk
As we already mentioned, ductus arteriosus goes through the process of elimination. This is enabled by the release of bradykinins from your lungs. During this time, the baby goes through withdrawal from its mother’s prostaglandins.
These chemical changes in the baby start the process of obliteration. This process might stop at some point, due to various disorders, thus enabling the ductus to obliterate.
You must take the utmost care of your child if you see the symptoms. Regular checkups are a good way to identify such a problem at an early stage.
If this disorder is not ruled out at the early stages, it might pose a greater threat to your child. It is always better to be safe than sorry!